Why supporting rapid intermittent flows is a core requirement from a blood/fluid warmer?
STEPHEN ALEXANDER
Stephen Alexander is a Critical Care Paramedic residing in Little Rock Arkansas. He enjoys writing informative and educational articles about pre-hospital medicine. Stephen started his career in EMS by enlisting in the Army as a 68W Combat Medic. He then attended the U.S Army Flight Medic program through UTHSCSA and received his paramedic license through NREMT. He then went to RUSH Advanced Trauma Training Program in Chicago and attained his CCEMTP. He currently flies for the Arkansas Army National Guard MEDEVAC unit.
In a previous article I discussed the top ten things you need to look for when choosing a blood/fluid warmer. In this article I want to talk about one function that, in my opinion, is absolutely necessary for your warmer to have and unfortunately completely overlooked. That is the ability to warm and handle intermittent flows.
Let’s start with a short background: most EMS service providers rely on gravity flow or pressure bags to try to infuse blood/fluids into a hypotensive patient. They might, if they were lucky, get a couple hundred CC’s into the patient before they arrived at the hospital. From there, if the physician determined that the patient needed a rapid bolus, the trauma team could utilize their rapid infusers in hospital. So why don’t we use the rapid infusers the trauma units have in EMS? Well they are simply too large (let alone that they are not battery powered). The model of rapid infusers that I have seen used are as tall as an IV pole and very, very bulky. This is fine when you’re in a trauma bay where space is a given. But in the back of an ambulance, space is a very limited resource. So an answer to this problem was introduced by handheld, push-pull, and syringe style infusers that allow for rapid infusion of blood products or fluids, in a matter of minutes, in an intermittent fashion.
So what exactly is intermittent flow? Intermittent flow is a term used to describe the flow of fluids generated by infusing devices such as the LifeFlow, hand pumps, and other push-pull style methods that infuse blood/fluids at very high rates and volumes and under increased velocity to patients in need. Some of the intermittent flow methods have been around for many years. However, newer intermittent flow infusers have been introduced recently, especially in the EMS world. This has to do, to some extent, with the continuous expansion of blood programs across the nation: EMS teams discover that transfusing blood fast to patients is often tricky due to the viscosity of the blood.
How do these devices operate? LifeFlow for example is using a 10cc syringe that can be reloaded fast to deliver a unit of whole blood (~500cc) in just 2 minutes. Some push-pull methods are using a 60cc syringe and a 3-way stopcock to achieve the same effect. Similarly, a recently introduced high-flow hand pump uses a 50cc squeeze chamber and wide trauma line to deliver the same results. The point here however is that irrespective of the method being used, all these handheld infusers are designed to deliver a large bolus of blood/fluids in a relatively short amount of time, and they are all capable of exceeding 200mL/min!
Further, unlike continuous flow, and as the name implies, intermittent flow starts and stops abruptly due to the nature of how fluids are being delivered. These rapid flows and intermittent patterns are extremely challenging for your blood/fluid warmer. Therefore, if your agency is utilizing intermittent flow devices, or if you are considering using such methods in the future, then I highly suggest that you are using a blood/fluid warmer that is up to the job. The QinFlow’s Warrior is one great example of a warmer that has been designed to meet this challenge, and I will address it in greater detail later in the article. For now, I would like to share with you some of the clinical aspects of intermittent flows.
So now that we know what intermittent flow is and how they are generated, let’s address the question of which patient population we as providers are going to utilize it on? Intermittent flow devices are used for the sickest patients. These patients are suffering from hypovolemic shock and need fluids/blood now! Think of the patient who has suffered from severe hemorrhage, or fluid displacement such as in septic shock, or a dehydrated hypovolemic pediatric patient. Patients that fall into these categories don’t have time for gravity flow, pressure bags, or even the highest flow rates that standard IV pumps can produce (most max out at 999mL/hr). These patients have already utilized all of their compensating mechanisms and by the time you arrive on scene to help them, they can be just minutes from irreversible, decompensated shock. These patients are the sickest of the sick patients we are going to see. So these patients are going to be treated with rapid IV fluid/blood bolus before it’s too late.
This presents a problem however. Do you think it’s a good idea to infuse a rapid bolus of cold blood products (stored at 4℃) into a hypovolemic trauma patient? Some of you may know the answer, but I’m going to explain why for those of us who might not know exactly why this isn’t a good idea. Let’s look at the trauma triad. It’s a triangle with three conditions on each side. They are; hypothermia, acidosis, and coagulopathy. When one side gets worse, it causes a chain reaction to make the other side worse, thus creating a vicious circle that results in death if not corrected.
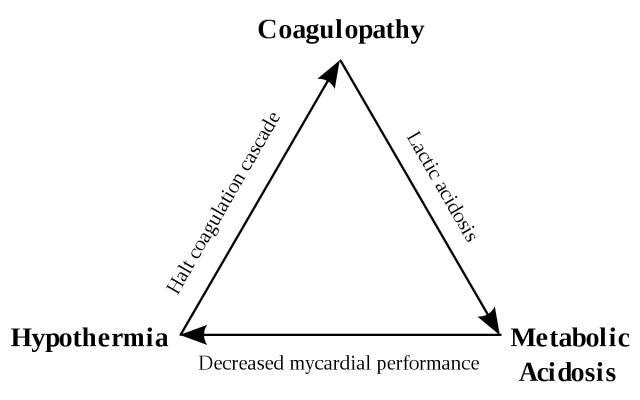
Let’s say we make the hypothermia side worse by bolusing cold fluids into a patient. In this scenario, I highly doubt that a provider would do this on purpose, however if you are using an inadequate blood warmer that can’t efficiently warm intermittent flows, you might do this unintentionally. How does this affect acidosis and coagulopathy? For every 1℃ in core body temperature, coagulation function decreases by 10-15%. Which means less ability to form clots and more blood loss. More blood loss means less oxygen delivery to tissues. Tissues deprived of oxygen revert to anaerobic respiration for energy production, a byproduct of which is lactic acid. This worsens the acidosis, which by the way also hurts coagulation and oxygen carrying capacity of red blood cells. Metabolic acidosis also decreases cardiac performance meaning less blood circulating in the body, triggering further hypothermia. Thus the downward cycle of death continues. All because we didn’t prevent the hypothermia side of the lethal triad.
However, when we warm the patient (via warm, rapid blood bolus), clotting factor activity increases, thus decreasing blood loss. Less blood loss means more red blood cells to carry oxygen to tissues. More oxygen to tissues means more efficient, aerobic respiration, and decreased lactic acid production, reducing acidosis. Correct the metabolic acidosis and your patient’s cardiac function will improve. Plus we are giving the patient blood products so more life saving red blood cells and clotting factors will be circulating in your patient!
So we can see that giving warm blood is absolutely essential in preventing the trauma triad! Better still when we can infuse those blood products via rapid (most likely intermittent) flow. But if we’re going to be rapidly infusing blood using intermittent flow, we need a warmer that is “smart” enough to recognize the intermittent flow pattern quickly, capable enough to warm those rapid flows, and responsive enough to stop the warming immediately when the infusion stops (i.e. this typically happens when the intermittent flow device reloads) so as to avoid overheating. And this process should go on and on until the transfusion is done. This is an extremely complex task for any warmer out there and not all blood/fluid warmers can deal with intermittent flows. In order to successfully handle rapid intermittent flows, a blood/fluid warmer has to meet four criteria. They are: real time temperature sensing, robust mechanical structure, high delivery rates/high efficiency, and optimal priming volume.
An example of a warmer that was validated to effectively warm intermittent flows is the QinFlow’s Warrior. The Warrior senses fluid temperatures hundreds of times per second. When a bolus flow is identified by the sensors, the Warrior’s highly efficient heat exchange process allows it to respond as necessary to warm the fluids to the proper temperature before being delivered into the patient. The heating will cease as soon as the sensors identify that the flow has stopped, avoiding overheating.
As discussed earlier, when using intermittent flow, your warmer also has to be able to handle the high flow rates that are pushed out by these methods. Intermittent flow mechanisms are capable of delivering more than 200mL over one minute, at high velocity! Having a warmer that can physically handle this elevated pressure is essential. If your warmer can’t withstand the high flow rates, it’s time to get a warmer that can. The last thing your patient needs is to have a warmer break in the middle of a blood transfusion.
Apart from physically withstanding the high flow rates and pressures of intermittent flows, your blood/fluid warmer has to be able to warm those fluids to body temperature just as fast. Whole blood is stored at 4℃ and needs to be warmed to 38℃ before entering the patient. At a flow rate of 200mL/min (or more), your blood warmer has to be able to perform this function. A critical part of warming fluids efficiently and adequately is to have sufficient priming volume. Sufficient priming volume allows the transfer of heat from the warmer to the fluids in a relaxed and incremental manner to ensure safe, yet rapid heating to match the high flow rates produced. The Warrior has a comfortable 19 mL priming volume which best fits the challenge of safely and effectively warming rapid intermittent flows.
I hope this article has shed some light on not only the importance of warming blood/fluids, but also how necessary it is that your blood warmer be able to handle intermittent flows. Fortunately, technology in EMS is ever evolving as we strive to better treat patients. Remember, you’re only as strong as your weakest link. The same goes for patient treatment. If your warmer can’t manage high flow rates and is the “weak link” in your treatment then it’s time to get a blood/fluid warmer that can.
It should not come as a surprise that the QinFlow Warrior can cope with the intermittent flow challenge. The engineers at QinFlow have roots in Israeli Special Operations and Search and Rescue. For decades these individuals have been coming up with solutions to save patients. Whether on the battlefield, natural disasters, or in civilian EMS, QinFlow’s experts have developed solutions with real world experience and application. The Warrior is one of their finest answers to solving the problem of blood/fluid warming in general and intermittent flow handling in particular across the entire continuum of emergency care. Irrespective of the infusion method used, from pressure bag to rapid intermittent flow methods, you can trust the Warrior to warm near freezing blood/fluids (4°C) to body temp within seconds! You can check out the Warrior and other solutions from QinFlow Here.