General
Warming Blood Makes A Difference for Trauma Patients!
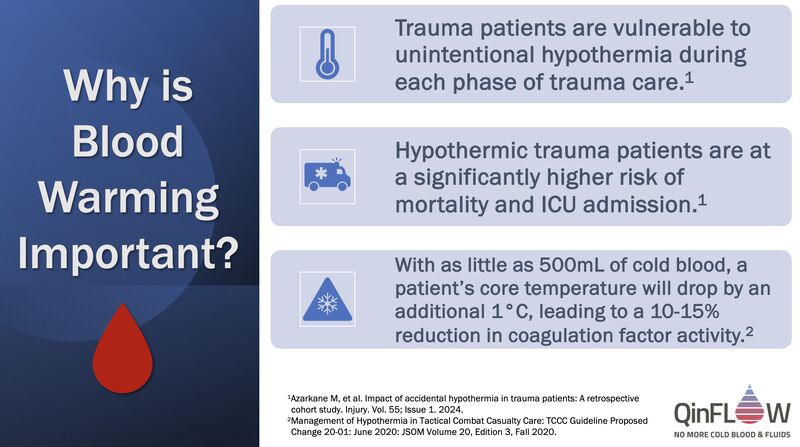
Hypothermia is common in trauma patients, with approximately 40% to 50% of moderate to severely injured patients arriving in a hypothermic state at civilian hospitals and >80% of non-surviving patients arriving with a core temperature <34°C (93°F).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7454138/, https://pubmed.ncbi.nlm.nih.gov/3656464/
With as little as 500mL of cold blood, a patient’s core temperature will drop by about 1°C, and coagulation factor activity will drop by approximately 10%–15% for each 1°C drop in temperature.
https://jts.health.mil/assets/docs/cpgs/Hypothermia_Prevention_Treatment_07_Jun_2023_ID23.pdf
Since the patient may already be hypothermic prior to initiating the blood transfusion, the adverse impact of cold blood is likely to be accelerated. As a result, it is not surprising that:
- Trauma Induced Hypothermia (TIH) mortality rates can be twice that of normothermic casualties with similar injuries.(https://jts.health.mil/assets/docs/cpgs/Hypothermia_Prevention_Treatment_07_Jun_2023_ID23.pdf)
- TIH is also associated with increased transfusion requirement, mortality, and ICU admission.(https://www.sciencedirect.com/science/article/pii/S0020138323006599)
Identified predictors for hypothermia included the severity of the injury, intubation, and immobilization, as well as winter season, SBP < 90 mmHg, and GCS ≤ 8.
(https://www.sciencedirect.com/science/article/pii/S0020138323006599)
Credit: Dr. Randall M. Schaefer (Lieutenant Colonel, US Army, Retired), DNP, RN, ACNS-BC, CEN